Extraction Defects: Should They Be Repaired Before Placing Implants?
Dr. F asks:
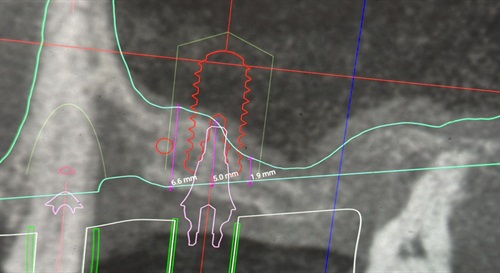
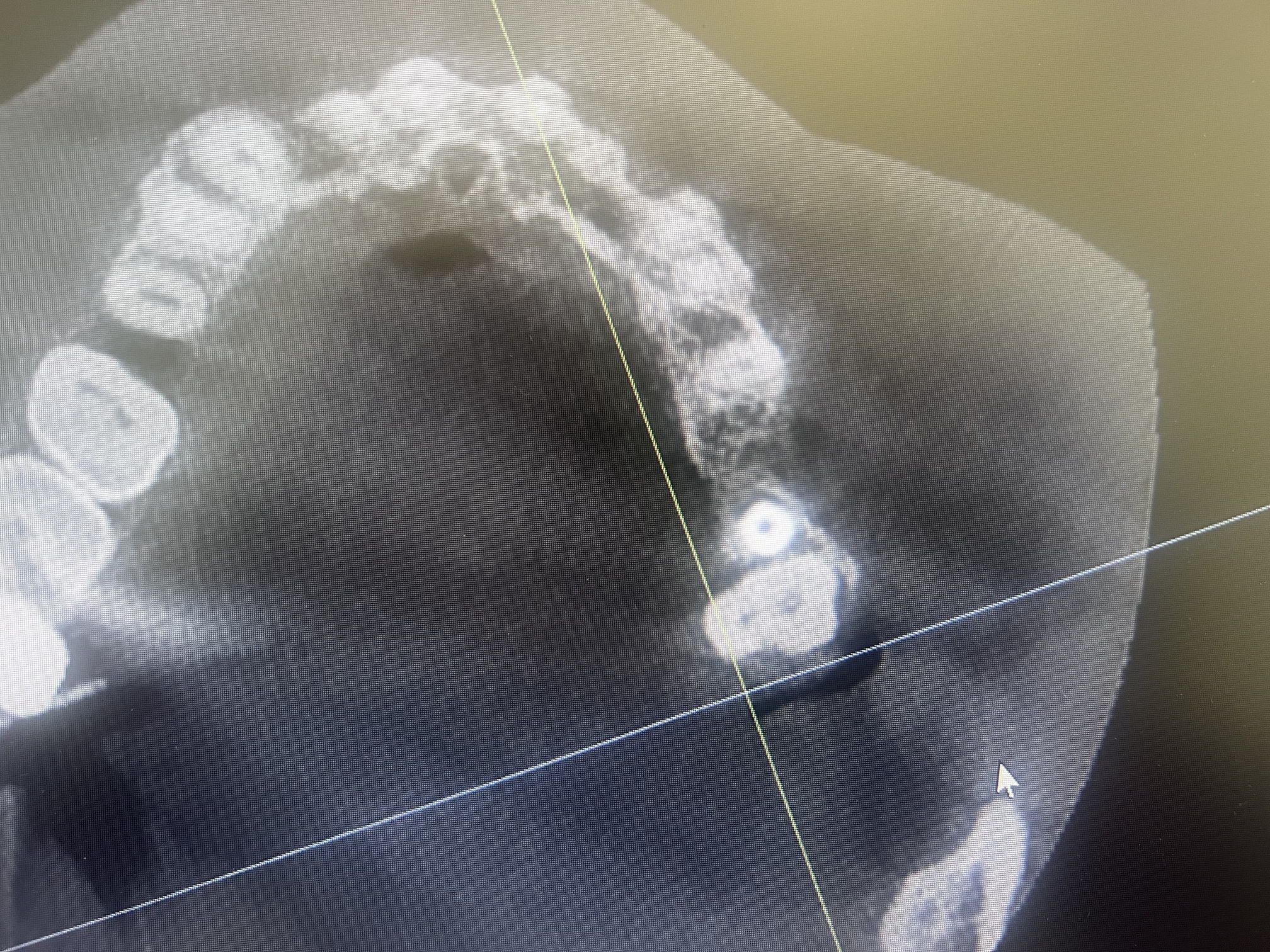
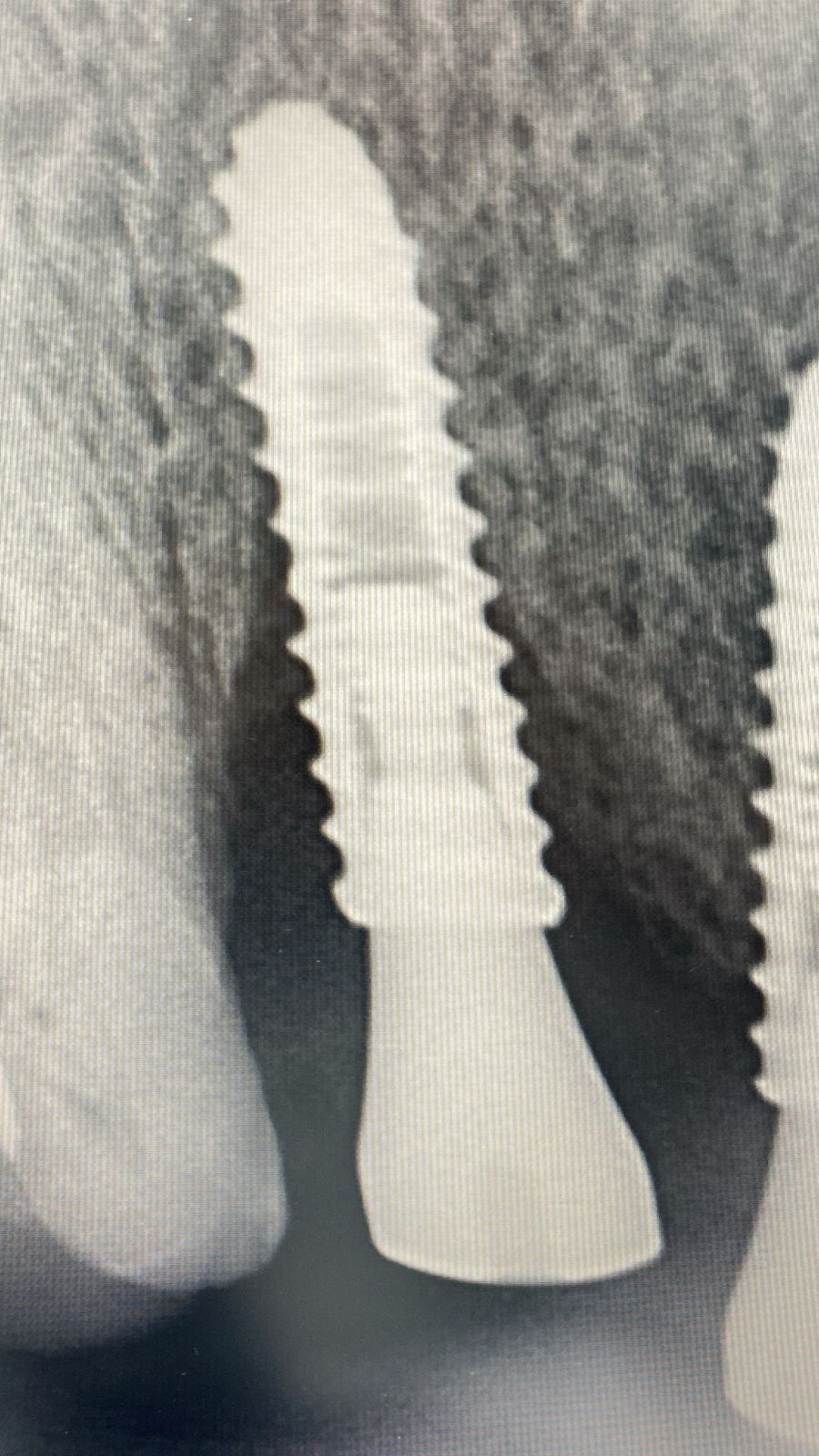
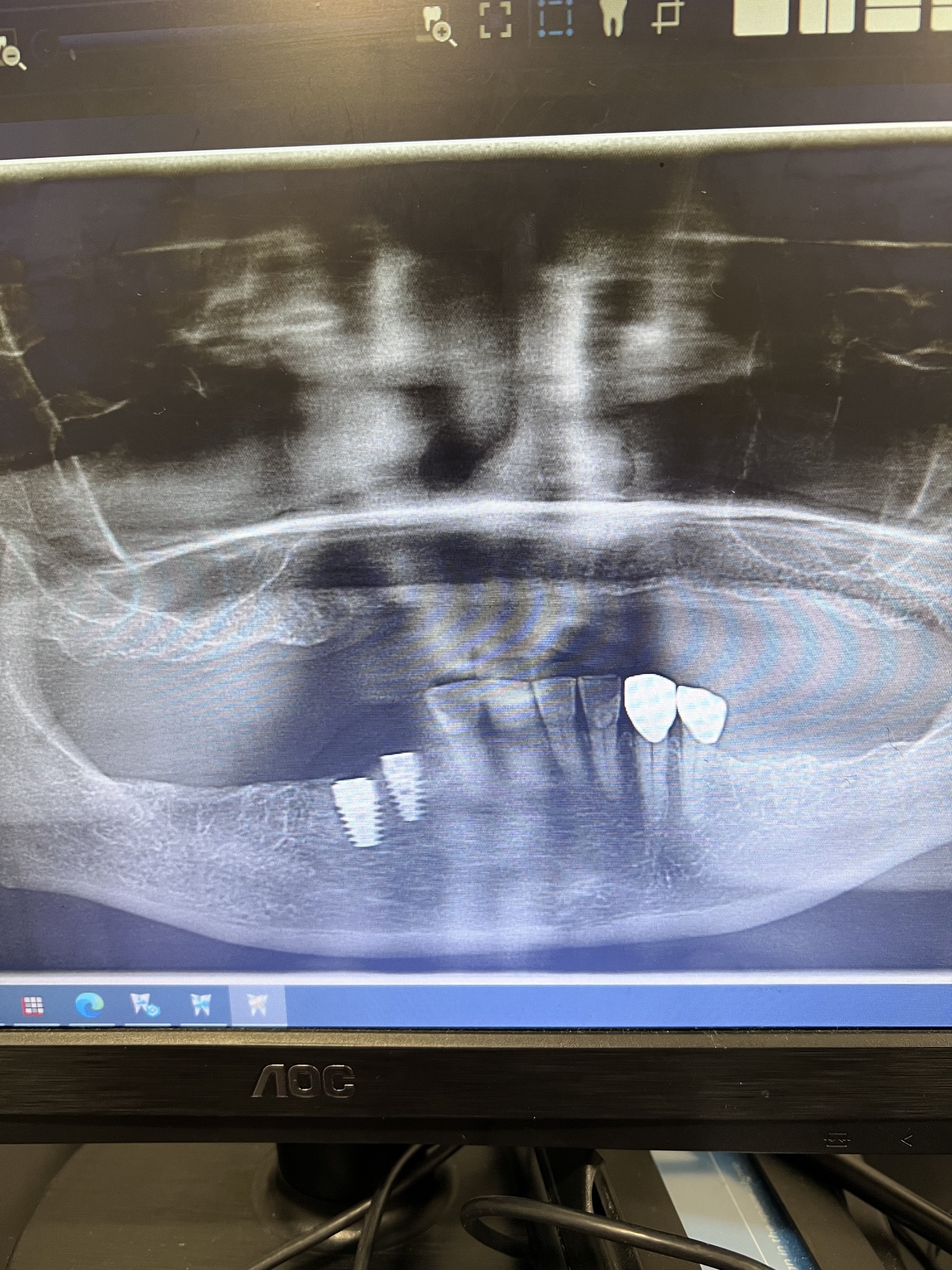
This rendered scan was taken 4 months after six anterior teeth were extracted. Should the extraction defects be repaired before placing implants? Should the implants have been placed at the time of extraction?

21 Comments on Extraction Defects: Should They Be Repaired Before Placing Implants?
New comments are currently closed for this post.
Le Oku
1/22/2012
No, you can place them now. Just make sure you pack some bone up in there when you do it.
david
1/24/2012
siultaneous placement with grafting can be done as long as implants placed into palatal bone and no pressure is on buccal bone . grafting now and waiting is an option and is easier for the novice. this case is not for the novice gp. david md,dmd.
david
1/24/2012
pack what type of bone.? bioss is non resorbing so when buccal plate resorbs, this material will be an intact wall to prevent further resorption. david
Dr. Alex Zavyalov
1/23/2012
Computer generated pictogram does not give us a real bone density image and generally speaking the situation is not favorable now for implant insertion without grafting.
Greg Steiner
1/23/2012
I assume the buccal walls were intact when the extractions occurred. If that is the case implants could have been placed at that time with grafting. What a nice display of why you need to graft extraction sockets. Now that the buccal walls are resorbing due to the lack of bone grafting I would do a ridge augmentation ASAP to reverse the resorption process. Remove all of the soft tissue in the extraction sockets and graft the sockets and place graft material over the buccal walls. Placing implants at this time will be unpredictable and the potential of integration on the buccal unlikely. With your permission I would like to use this image in my grafting seminars.
Greg Steiner Steiner Laboratories
fred firth
1/24/2012
Hi Greg
Please feel free to use the image.
Don't know if email addresses are allowed here, but if they are, I can send you the L/H & R/H images also.
Greg Steiner
1/24/2012
Thank you very much Fred. My email is ggsteiner@steinerlabs.com. If for some reason that is blocked you can email me through our Steiner Laboratories web site. Thanks again Greg Steiner
peter fairbairn
1/24/2012
Great Points above , I generally do a slightly delayed ( 3 weeks ) in these cases to help with soft tissue closure which can improve the result. Otherwise exactly as Greg says it . It is a nice picture to show the effects but again as Alex said an estimation.
Peter
SG
1/24/2012
An important factor in this case is what are the esthetic considerations? This is to say, that if esthetics are a concern, then immediate implant placement is not advisable as the level of the soft tissue is subject to variability following the placement of immediate implants. If this is the case, I think grafting either right at the time of extraction, or several weeks post extraction as suggested above are the treatment of choice. If, however, esthetics are not an issue, then immediate implant placement would have been fine, with some additional grafting on the labial surfaces.
DrT
DrS
1/24/2012
I think that it has become clear based on Tarnow's work and others that, if at the time of extraction, there is no buccal bone, then immediate implants are contraindicated. Careful evaluation of the buccal bone at the time of extraction guides you in decision-making. If this represented the buccal bone at the time of extraction, then I would have undermined the mucosa, placed a resorbable membrane and grafted the sockets with a granular cadaveric bone material (just my choice of graft).
It also depends on your goals. Is it multiple implants and a fixed prosthesis? Is it all-on-4? Is it 4 implants and locator attachments? The ultimate destination should allow you to develop your roadmap.
gerald rudick
1/24/2012
Dr F asks for answers without giving us adequate information.
Why were these teeth extracted?
Were these teeth abscessed at the time of extraction and did the lesions work their way through the labial plate?
What other information can be be gotten from the scan?
It is best to have all the information at hand before taking a decision whether to graft and wait before placing implants,etc.
Remember Lte. Joe Friday of Dragnet " The facts, Mam, just the facts!"
Gerald Rudick dds Montreal, Canada
fred firth
2/1/2012
Dr Rudick, Teeth were not abscessed or loose. Removed to facilitate All-on-Four (or 6). See part 2 of case, here on OsseoNews. Plenty of images and details. Your comments will be appreciated.
ttmillerjr
1/24/2012
I think you'll find the buccal bone is in better shape than the image suggests. Why don't you assume it is as it looks. Plan to graft the areas and open a flap. This will be a real learning experience, you'll have a better idea of how to manipulate the contrast to more accurately represent real conditions.
E Katch DMD
1/24/2012
As far as what should have been done initially, it really depends what your goals, the patient goals, and expectations are for the end result. Fixed/Removable? Immediate load? How are you provisionalizing? Esthetics? Biotype? Age of Pt? Bruxer? Just from your question it seems you are jumping in over your skill and experience level. When in doubt, graft and wait, is probably the most tried and true approach. You should really be working this up with the end result in mind, and at least a lab consult, and probably a consult with a clinician whom you respect.
Juan collado dds
1/24/2012
It is best to graft bone for recontour the alveolar bone ,especially in buccal.wait for it after 6 months,for better placement of the implants and the restoration .
fred firth
1/25/2012
Oops, sorry everyone. I was creating a set of instructions to help a computer-shy dentist to post this case, but when capturing the image of the submit button, I accidentally submitted it using my name.
The image and heading “Extraction Defects: Should They Be Repaired Before Placing Implants†was actually the first of several. I didn’t think I should send the rest of the images and info until I had permission, which I now have.
There seems to be quite a lot of interest, so if the moderator is agreeable, I will send the rest tomorrow under the Heading Extraction Defects Part 2.
osseonews
1/25/2012
Yes, you may post additional photos, by clicking on the Post Case photos link at the top left of the website. Here is the link: http://www.osseonews.com/post-case-photos-and-get-feedback/
Be sure to reference the current case and use the same email you used to post the first case photo. Thanks.
fred firth
1/26/2012
Thanks
I have just posted
Dr Sumeet Sherwani
2/4/2012
I would assume that Buccal walls were intact when you extracted the anterior teeth. If I had even 3 to 4 mm depth of extraction socket I would have gone for BCS implants from IHDE DENTAL. It works wonder in lower anterior teeth. You can place upto 17mm of implants. It engages cortical bone and initial stability is more than 40 Nw most of the time. I think for lower anteriors which are periodontally involved and mobile, extract them and place two BCS IMPLANTS...most of the cases do not need grafting, even if grafting is needed its only on Buccal defect. Patient walks away with temporary bridge immediately post extraction and placement of implants...
Richard Hughes, DDS, FAAI
2/4/2012
This depends on the available bone and the relationship to vital anatomic structures. It is always safer and easier to graft and revisit. See the post about bagging the IAN. This is one for grafting first.
greg steiner
2/6/2012
It may be worthwhile here to talk about why the buccal bone resorbed. In middle aged and older people the interproximal and lingual bone is maintained but the buccal bone becomes thin and loses all trabecular bone and we are left with only a buccal cortical plate over our buccal roots on bicuspids and incisors. When you extract and don't graft the bone lining the socket dies and osteoclasts migrate in the tubercular bone under the dead bone, undermine the dead bone and separate it from the live bone and the dead bone is released into the socket. The bone on the buccal wall has no trabecular bone for this process and the complete buccal wall dies and is lost as in the ct scan. The next question is just because the buccal wall dies why does the socket still not fill with bone? The reason is that trabecular bone will form in a hole (socket) but cortical bone will form on a surface. When the buccal wall is gone the mesial, distal and lingual walls become a surface and cortical bone forms on these walls and no bone forms in the original socket. While these principals hold for all patients every patient presents with a different clinical situation and being able to asses a patient and prescribe a predictable treatment plan makes regenerative therapy fun. Greg Steiner Steiner Laboratories