What is Standard TX plan for Maxillary Full Arch Implant Restoration?
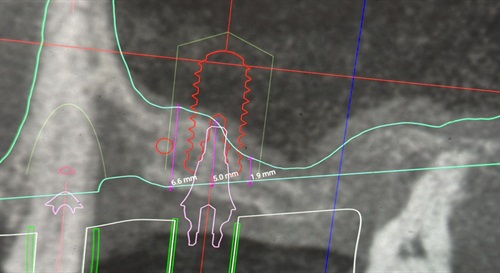
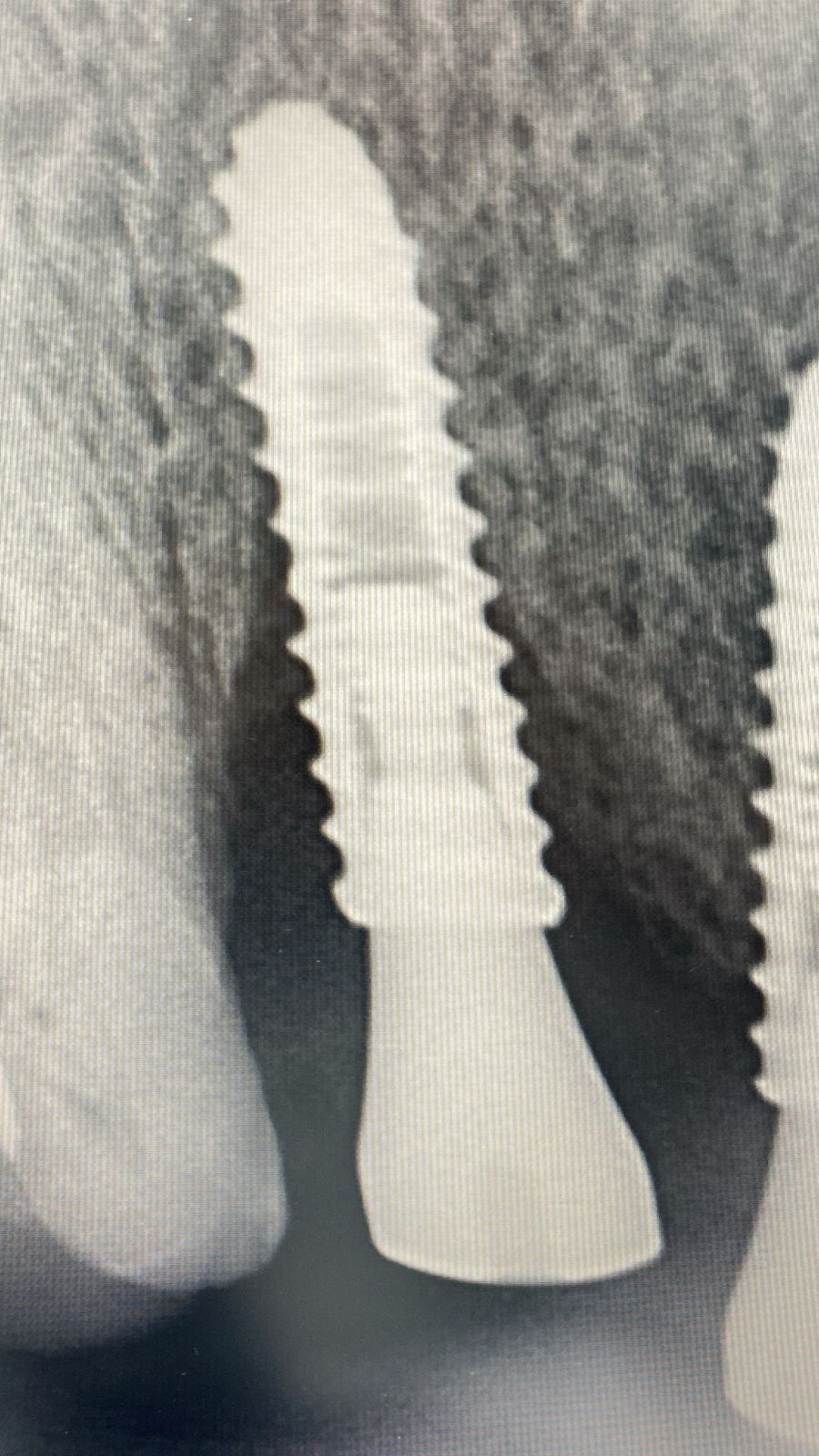
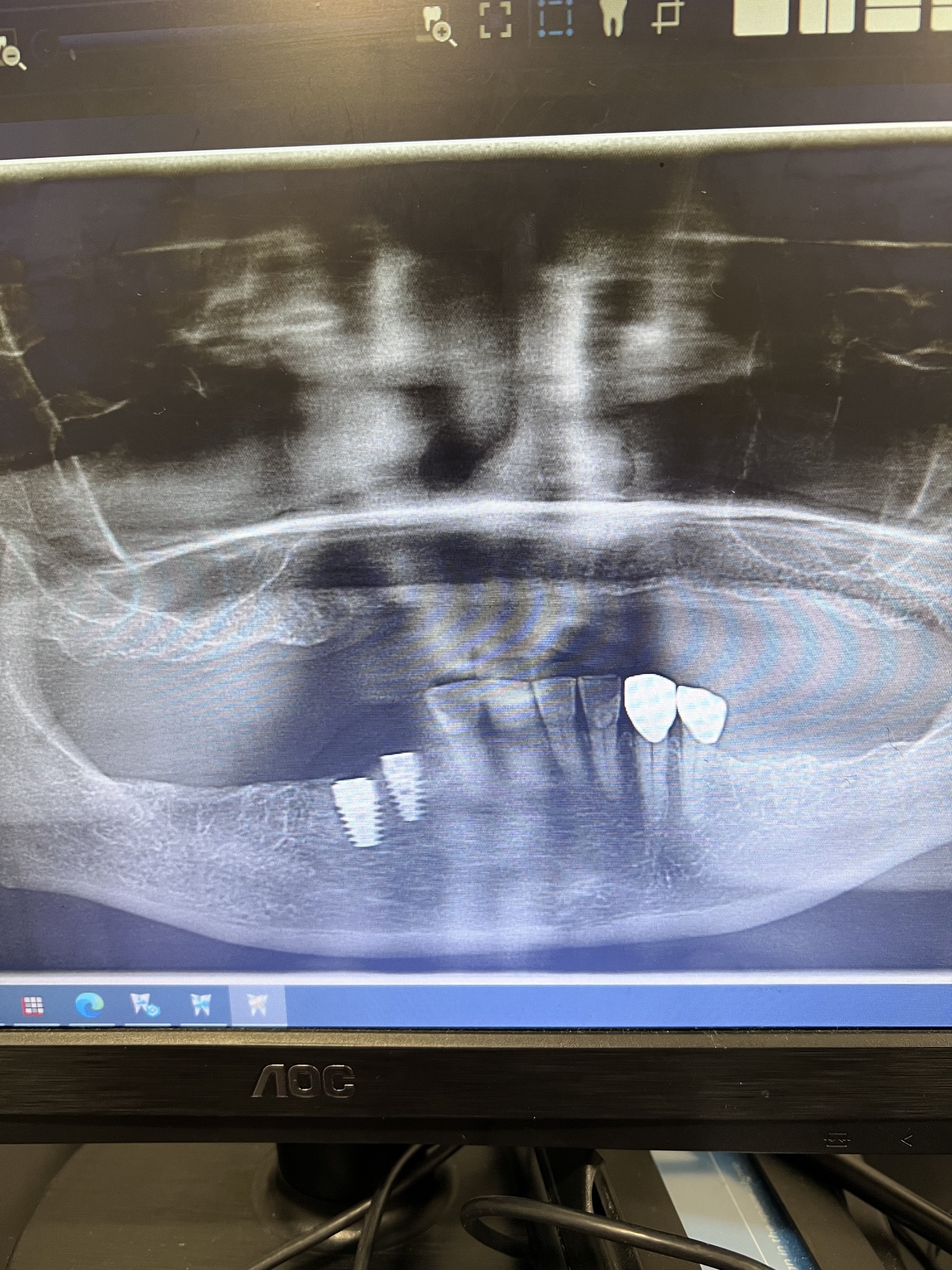
I have treatment planned this patient for maxillary arch reconstruction using 6 implants and 3-fixed partial dentures. Install implants in #6 and 11 sites [maxillary right and left canines; 13, 23] to support anterior 6-unit FPD. Implants in #2 and 5 sites [maxillary right second molar and first premolar; 17, 14] to support 4-unit FPD from #2-5. Implants installed in #12 and 15 sites [maxillary left first premolar and second molar; 24, 27] to support an implant FPD from #12-15. Will do sinus lifts as needed. Thoughts on this case? Any advice appreciated

27 Comments on What is Standard TX plan for Maxillary Full Arch Implant Restoration?
New comments are currently closed for this post.
peter Fairbairn
8/14/2014
Looks good case lots of bone ( without CT cannot tell width ) . If want fixed then best to use 6 or even 8 Implants and cross arch splint ...
Can use the tuberosity areas as well as looks good bone there .
A fixed arrangement may lead to issues with the minis on the lower later , but then patient may want fixed lower ( There use 3 separate bridges ) after having the benefits of the fixed upper ....
Peter
ben manzoor
8/15/2014
Sounds like a good plan.Hopefully u be able to provide screwretained restoration?
CRS
8/16/2014
I would advise eight implants making sure the first molar and canine areas are covered. The second molar regions are not critical, I would go with first molar occlusion. The minis will need to go in the future but can support an interim prosthesis. Full wax up with face bow and appropriate surgical guides for both arches. Start with the maxilla. Keep the bridges separate for hygiene. Unless the ridges are narrow there is plenty of bone. If it were me I would treatment plan with Simplant with the radiographic stent fabricated from the wax up. Now here is the key with this blueprint you can change up the treatment if there are financial issues, fixed bridges anterior, locator supported posterior. I would not try to eyeball the implant placement a good work up is key. This is an advanced case with fixed.
sharon
8/26/2014
Hi CRS!
I like the suggestion you alluded to of implant bridge anteriorly and Locator implants posteriorly.Would you do a fixed bridge say #6 to#8 to #11 and then say Locators #3#5 and 12 #14 to retain an Co Cr RPD with a broad metal U shaped palate in the interim?
Thank you !!
CRS
8/16/2014
Also needed to mention the soft tissue, lip line and transition line for esthetic will any pink porcelain be required for phonetics and esthetics. It is often overlooked in these cases and the final result is crowns that are too long trying to adjust the inter occlusal space. That's why is is important to take into account the mandibular arch and vertical dimension. You can use minis in the upper to support the interim prosthesis or immediate load the upper if the insertion torque is good and the temporary is all one piece with cross arch stabilization. It's like an all on four with plenty of bone but the abutment type is very important to adjust any discrepancies.
Richard Hughes, DDS, FAAI
8/16/2014
I use a modified Ante's Law principle. I take the number of teeth to be replaced and divide by two and add one. This gives me the number of implants. I know some people segment the cases but I like to cross arch stabilize as Peter suggested. The lower should be segmented when possible.
Occlusal control and hygiene are paramount for long term success. However when in doubt, upper and lower bar retained overdentures work very well.
MMontana
8/19/2014
Mini implants do not support prostheses, they retain them. Therefore, reconstruction of the maxilla will likely result in excessive pressure of the mandibular soft tissue. Over-dentures are supported by the residual ridges and are thus biting force is limited by feedback from these tissues; they don't allow themselves to be crushed. Personally I'd rather reconstruct a lower arch if a patient can only afford one jaw. Lower fixed versus an upper denture is certainly reasonable as the tough tissue of the palate resists greater pressure than the posterior mandibular residual ridge.
Mcfat
8/19/2014
Cross arch stability. You will be cantilevering the incisors so if have a tapering arch form may need an anterior implant. Also the further back the terminal implants will give better AP spread in poor bone. 1st molar occlusion but can have implants distal to the 1st molar Good luck
Tuss
8/20/2014
If you stick with a lower implant overdenture then you will have better control over occlusal loading. Best to work up the case with a denture set up to see where your teeth are going to be relative to the residual ridge and then decide on fixed, bar over denture. If you need a lot of lip support then a bar OD will give you the best aesthetics plus from a hygiene point of view easier for patient to clean around the implants. Side note - angluation of lower implants looks a bit suspect if you are using ball attachments longterm
Ernest
8/20/2014
Before suggesting a possible solution I would like to know how long the patient has been wearing dentures, why were minis used in the lower and how long they been there. In this pano they look good. Did the patient request implants in the upper because the improvement in function of the lower due to the minis? Does the patient want to eliminate the palatal coverage? Is cost a factor and, if not, why weren't conventional implants used in the lower. Has the patient been advised as to the cost of the maxillary treatment plan?
I agree that fixed above may jeopardize the longevity of the the lower restoration. If the patients only complaint is an unstable FUD and considering the quantity of the maxillary bone I would place six maxillary minis. This is presented as an option.
If money is unlimited, in my opinion, a cross arch stabilized conventional implant supported upper and All On Four lower would be the best solution.
It would be very interesting to see what the results would be with the original plan.
nailesh gandhi
8/20/2014
I endorse views expressed by CRS & Richard Hughes. Since 27 years we are doing maxillary planning with steps explained by both the experts.Our experience says the bridge shall be crossarch and not segmental in maxillary case.Screw retained is preferable.
Jalil Sadr, DMD, MSD, FIC
8/20/2014
Hello to all. Most agree with Drs. CRS and Richard Hughes.
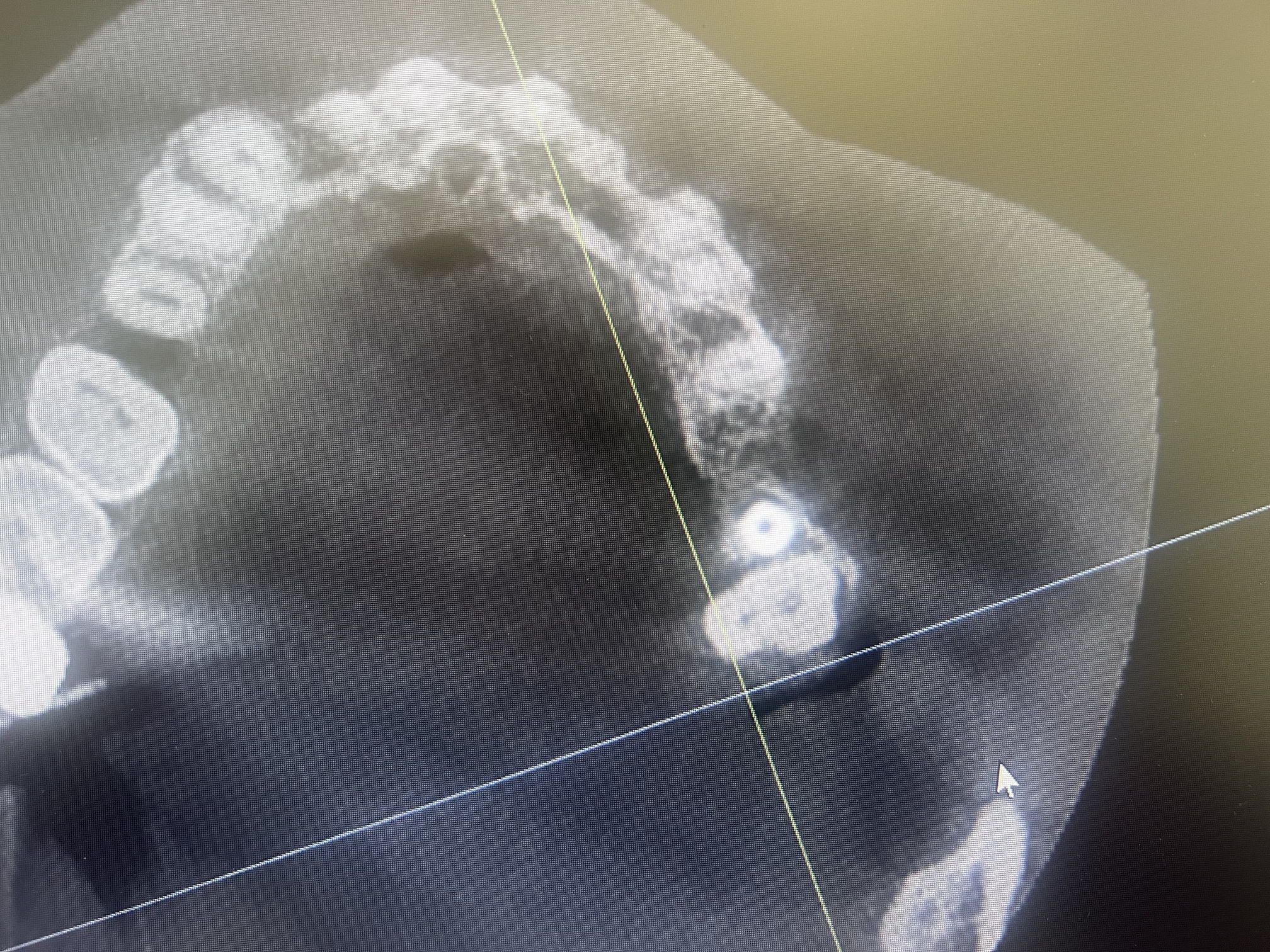
Patient sex and age did not mention. But good bone height even in sinus area as OPG shows. CBCT is needed for width and ...
However, TX for this Pt could be:
1- Full upper and lower denture, to see function and esthetic, and ... evaluations
2- Fabrication of Radiographic Guide for CBCT. and then
3- Surgical Guide
4 - Implant Placement; Considerations: No Cantilever, No more than three pontics, and Cuspid and Molar rules according to arch form and bone width and imolant diameter and lenght and ...
A: 6 implants ; 2 in Upper Laterals, 2 in Cuspids, and 2 in 1st Molars
area ( Bt 2nd Bicuspid and 1st Molar)
B: 8 implant 2 in Upper Laterals, 2 in Cuspids, 2 in 1st Bicuspid and
2 in 1st Molars area
C: More than 8 9 or .. more sections the better.
thank you
sharon
8/26/2014
Hi Jalil; I like your treatment suggestions in terms of implant placement.If you are doing a full arch splinted restoration on 6 or 8 implants do you try and aim for a screw retained superstructure for retrievability? Do you have problems attaining a passive fit or are the CAD CAM frameworks so accurate that even in multi implant cases this is not an issue anymore? BTW in the 8 implant scenario you mentioned what does Bt stand for? Thank you for sharing your knowledge with us!!
mwjohnson dds, ms
8/21/2014
As a board certified prosthodontist I can assure you there is no such thing as a standard maxillary treatment plan! One of the most difficult treatments in dentistry is the fully edentulous maxilla. Most of the commenters have touched on points to be aware of i.e. Lip line, lip support, number of implants, implant positions, materials selection, tooth shape, position... and the decision tree goes on and on.
There was no discussion as to whether you are a restorative dentist or surgeon. What is your skill level? This is an incredibly difficult restoration. Implant placement (with any luck) is forever so difficult to fix if something goes wrong.
However, here are my thoughts. If you want to do a ceramometal restoration then there needs to be adequate bone for lip support without a flange and adequate ridge size so the teeth don't look too long (cosmetic issue). I usually ask for 8 implants to make four 3 unit fpds, 3-5, 6-8, 9-11, 12-14. That way they can be screw retained if needed or cemented. Trying to achieve a passive screw retained one piece full arch ceramic restoration on multiple implants is difficult and porcelain doesn't like to be torqued; it will break.
If you are doing a resin based fixed restoration then I generally make it in one piece using 4-6 implants evenly spaced throughout the arch form since angled abutments can be used to reorient the screw access holes. Implant position and angulation is less critical with a resin based fixed prosthesis. With a fixed prosthesis, a flange cannot be used. If lip support is needed, a bar/clip overdenture can be made with the same implant numbers and positions as a fixed restoration. If going with a resin system you will need plenty of interarch space for the bar. Do you need to remove alveolus to create interarch space?
I agree with Dr. Montana. What are your thoughts with the mandible? You run the risk of overloading the lower implants. Also, if the ultimate plan is an acrylic mandibular overdenture then having a similar material in the maxilla may make sense.
As you can see, the maxilla is not simple. It may be wise, if you have never done one, to enlist local specialists to help you, or refer to them and watch what they do before trying one of your own.
Best wishes and good luck!
Richard Hughes, DDS, FAAI
8/22/2014
Dr Johnson,
Very well stated. Thank you.
sharon
8/26/2014
Dr Johnson that is an awesome response! Thank you so much for sharing your expertise with us!! With the advent of CAD CAM technology how low profile can you go for a bar for a bar retained overdenture? Do you like to use the milled bars with a secondary superstructure for precision fit or do you like to have resilient attachments like Locators on top of the bar or Bredent attachments offset lingually to save on space?
Do you like to leave 1mm of space below the bar for cleansibility or do you find that causes more tissue hypertrophy?
Even if you can use a lower profile bar and maybe not leave the 1mm space for cleansibility, what is the minimal amount of space you have used from the fixture level to the opposing occlusion for a bar retained prosthesis?
Thank you your valuable input!!
nailesh gandhi
8/26/2014
For mutiunit splinted full mouth bridge we have used screw retained since years for retreivibility With cadcam technology passivity is sure good and fitting is precise.
mwjohnson dds, ms
8/26/2014
Hi all;
thank you Dr. Hughes and Sharon for your kind words. In answer to Sharons question, CAD CAM bars are great. You still need at least 1.5 cm between the ridge and the opposing dentition to have enough space for hardware and teeth. Make sure, in a full smile, the ridge is not visible. I have used the "spark erosion" technology that theoretically doesn't need clips. It worked well but now I use hader clips anteriorly and the large bredent ball attachments off the distal of the bar posteriorly. This keeps the vertical space from getting filled up with attachments on top of the bar (locators etc). I then overlay the bar with a superstructure for strength and rigidity then process the teeth to the superstructure. I prefer the newer composite based teeth like Ivoclar Phonares or the Bredent denture teeth for added wear resistance.
Hope this helps!
mwjohnson dds, ms
8/26/2014
oops, to answer your second question, I try to leave some space for hygiene but it invariably gets filled with hyperplastic tissue. I haven't figured out how to eliminate the hyperplasticity, even with perfect home care. If anyone has any thoughts I would be interested in any ideas.
sharon
8/26/2014
Thank you Dr Johnson for the speedy reply! Talking about space calculation from the ridge am I right to assume the soft tissue ridge or the hard tissue alveolus? am just thinking about the diagnostic phase when you look at casts on an articulator. if it is the soft tissue then we have to really calculate at least 17mms from bone to the opposing occlusion to guide alveolectomy...15mms to the bone like what is quoted often would not really be enough!
Why do you prefer a hadar clip and bredents vs spark erosion? I have not used clips before but understand they need regular replacement? Thank you again for your input!!
mwjohnson dds, ms
8/26/2014
15mm from soft tissue to opposing occlusal surface is, in my mind, the minimum distance and the more the better. I like clips vs. spark erosion for several reasons. Spark erosion refers to a technique for precisely milling a bar and superstructure. It is very expensive from a lab perspective and there's minimal adjustment available to compensate for wear of the metals over the years. Yes, the clips need replacing but if the clips simply retain the superstructure to the bar there is less force to the clips; i.e.no rotational forces, so they only need replacing every year or so. As the metal wears (which it always does) then there are females with greater retentive strength that can be used. I like the flexibility of adding or subtracting retention as needed (someone with poor hand strenght gets weaker clips etc) which is not available with the spark erosion technology.
sharon
8/27/2014
Hi Dr Johnson.Thank you so much for taking the time to write such comprehensive answers. We are fortunate to have someone with your extensive experience to answer our queries! Its interesting because I went to the ACP implant review meeting last November and one of the speakers was saying that he does not any resilient attachments on a bar borne prosthesis and prefers everything to be rigid and friction fit like the spark erosion technology will give. I have seen case reports where Locators are placed on top of the bar but this obviously requires extra space! I guess different clinicians have varying preferences.
What is interesting and relieving to note is that you like to break up a fixed restoration into smaller units for ease of cementation/screw retention. Do you think with the advent of implants with improved surfaces there is less need to splint multiple implants together? If you are dealing with grafted bone or shorter implants say 10mms in length, would you splint across the arch and use precision attachments to assist in breaking the case up, to assist in achieving a passive fit?
I know there are mixed views regarding the use of 4 unsplinted Locator attachments retaining a U shaped/palateless denture maxillary denture .I was just wondering with your level of experience what your thoughts are about this type of treatment? Thank you very much once again!
Best wishes
mwjohnson dds, ms
8/28/2014
There are newer conus type abutments that are friction fit like the "spark erosion" technology and are interesting. They retain via friction as well. They are individual abutments and the female "cone" is picked up chairside to assure a passive fit. They are by dentsply and called the syncone abutment. The "spark erosion" technology is getting harder to find, from a laboratory perspective. Dental Arts in Illinois was one of the primary labs making the bars. That's why I like attachments, they can be milled or cast and are not necessarily lab intensive.
In regards to shorter implants, I actually consider a 10mm implant as sort of a normal length these days. With the active surfaces it seems rare to place an implant much longer than 13mm. Many companies are coming out with 6 and 8mm implants and I would now consider these as the short ones. Splinting always depends on the force to the implant. If you're using several 6-8mm implants to dodge a sinus or nerve then I would splint them. Likewise, if the implant is primarily in grafted bone (i.e. sinus aug with less than 5mm of host native bone) then I might tend to splint. This topic is open to discussion and there are many opinions on the subject. I tend to lean towards overengineering since I hate failures. Also, if you're doing a big edentulous fixed case and you have multiple pontics in a row it might be better to cross arch stabilize to decrease the force to each individual implant. That's the tough part. It's hard to predict when an implant will be overloaded. There's so many variables; Bone density, length of implant, length of span, power of occlusion etc, etc. so I tend to overbuild. When in doubt make it stronger.
In regards to the four locators in maxilla, I don't do it. The maxilla flares so the implants will flare facially too. The path of insertion then becomes an issue. Plus, most of the time these locators are placed from cuspid to cuspid so the denture has to rest on the residual ridge. With function, the prosthesis will fulcrum around the posterior implants and cause the anterior locators to pop loose. Gets frustrating for me and the patient. I know practitioners do this and I'm not saying it's wrong but, as I have said, I'm a chicken and want to overengineer. Our patients are spending a significant amount of money and the surgical placement of implants is at least half of the cost. Therefore, with four implants fabricate a bar to splint them together. You can spread the attachments out more and create a more stable prosthesis along with guarding the implants against overload. The palate is the primary denture bearing foundation of the maxillary prosthesis and when you remove this, the forces are directed entirely to the implants so make sure there's enough inherent strength of foundation to support this force.
As you can see, the maxilla is a challenge!
sharon
8/28/2014
Thank you Dr Johsnon again for a great reply!
Best wishes,
Sharon
naileshgandhi
8/28/2014
Maxilla is a great challange indeed !
Bill M
9/25/2017
I think you should reconsider this Tx plan. As cautioned above, you will over load the mandible and then you may have a great case for pictures and a pat on the back but a non-functional case. If you take to time to consider the occlusal set up for the patient and where the forces are you know these forces are in the posterior which will be supported with the lower ridge Anyone that does dentures knows that the lower is difficult when an upper denture is the occluding prosthetic . Now you want to put a rigid structure hitting in the posterior on this ridge -you will destroy it further and you will have pain. Do yourself and the patient a favor and get full support on the lower first before you do the upper case with implants or you may need to bury the implants for the patient to eat
Nailesh Gandhi
9/26/2017
How about an all on four with plenty of bone in this case or such cases. ?